Why did I chose to discuss this injury?

I have a lengthy history of injuries in my athletic career but none has taken a toll on me more than Patellar Tendinopathy. I have suffered from a torn MCL, torn meniscus, severely sprained ankles, hyper-extended elbows, dislocated fingers, a concussion, and yet my Patellar Tendinopathy has affected me the most. In the picture above my teammates are carrying me off the field after I tore my MCL and meniscus in my first year in the CIS (Now USport). At the time I felt this would be the most significant injury I would suffer. I used to laugh when my little brother said his knees hurt from playing basketball. Slowly I started to develop a dull, achy pain in my knees that lingered after activity. It then developed into a sharp pain before, during, and after activity. It hindered my performance as I was not able to play “low” enough which is ideal for offensive lineman. My positional coach constantly said “Ed you go to get lower!!” little did he understand It physically hurt to play “low”. I constantly imagine a career without suffering from Patellar Tendinopathy. How much faster would I be? How much more powerful would I be if I played lower? How much stronger would I be if I was able to Squat properly and pain free?
What is Patellar Tendinopathy?
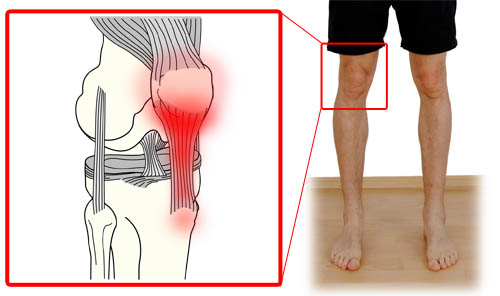
It is an overuse injury affecting your knee due to the Patellar tendon being frequently being stressed. It is commonly referred to as jumper’s knee, or Patellar Tendinitis.
Where is Patellar Tendinopathy most common?
For the most part it is found in jumping athletes such as Volleyball and Basketball players. It is also seen in individuals who repeatedly put their knees under load due to training such as runners, football players, and power lifters
Mechanisms of Injury
Training Errors. A rapid increase in intensity, a change in surfaces, or an increase in training frequency may lead to Patellar Tendinopathy
Poor Flexibility. Tight quadriceps, tight ankles, tight hamstrings contribute to Patellar Tendinopathy
Lower Limb Biomechanics. Poor foot posture, inability to activate glutes, patellar tendon not tracking properly, muscular imbalances
Signs and Symptoms
- Pain in knee gradually getting worse over time.
- Stiffness in night and morning.
- Tender area may be warm, swollen, red.
- A crunching sensation, and sound.
- Movements like walking up stairs, or standing up hurts.
Complications
Complications that commonly occur with Patellar Tendinopathy are athletes playing through pain. Athletes are notorious for playing through pain. Patellar tendinitis starts off from mild and gradually increases in pain, so athletes just get use to playing with it. If no action is taken the tendon begins to tear over time and surgery may be required.
Stages
- Reactive tendinopathy
- Normal tissue adaptation.
- Tendon disrepair
- Vital you prevent deterioration and progression.
- Degenerative tendinopathy
- Cell death occurs.
- Tendon tear or rupture
- Tissue is broken down.
- Loss of function.
- Surgery may be the only option at this point.
Management
Rest. Avoid any activity that makes the pain worse as best as you can.
Apply Ice. Reduce swelling and pain by icing in 20 minute intervals at a time.
Maintain Range of Motion. Stretching and gentle range of motion exercises are important to prevent the individual from being rigid.
Assess movement patterns. Treating pain is important but you must address the source of the pain with a specialist.
Clinical test
X rays, Ultrasound, MRI.
Treatment for mild Patellar Tendinopathy (Stage 1)
- rest until pain is gone.
- improve biomechanics to reduce load on tendon.
- reduce training load and intensity.
Treatment for Patellar Tendinopathy for Stage 2-4
- Resting here does not completely heal the tendonitis.
- Optimize diet to improve healing.
- Implement strengthening program.
- Improve flexibility in problem areas.
Benefits of goal setting in rehabilitation
- Create a sense of purpose.
- Focus on what’s important. Focus on the now.
- Increases your motivation.
- Make better use of time during rehab.
Goals for each stage in rehabilitation

Psychological issues that may occur during injury and rehab

Fear of unknown. Individuals do not know how they will perform once they return to play. They fear they may never regain their pre-injury performance levels. Individuals also fear having their spot taken by a teammate.
Boredom. Not being engaged with the team, along with physiotherapy may become repetitive causing the individual to not invest effort into the rehabilitation process
Isolation. Individuals may feel left out from team the environment due to inability to participate in practice an/or games.
Coping resources to deal with psychological issues during rehabilitation.
- A solid social support system (team, coaches, family, teammates, coaches physicians, rehab support group, and friends).

Senior Laurier football players with parents, along with teammates.
- Use of healing imagery.
- Deep breathing techniques.
- Yoga to improve mental and physical.
- Talking with individuals who have gone through the same injury.
- View injury rehab as process as an extension of sport performance, rather than a grueling task.